Fighting Neurodegeneration
When patients have Parkinson’s disease, for example, and are not responding well to medications, they can undergo surgery to receive an implanted “deep-brain” stimulator (DBS) in the subthalamic nucleus. The device produces a steadily oscillating electrical field to “pace” what would otherwise be erratic and excessive oscillations. This restoration of rhythm can curb symptoms such as tremor.
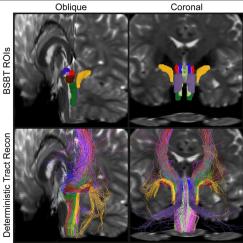
But Dr. Diane Chan, a clinician at Massachusetts General Hospital and Brigham and Women’s Hospital and a researcher in Tsai’s lab, notes that because surgery and implants carry risks such as infection or stroke, the treatment is restricted to patients with urgent need. That’s why she is excited to test a new non-invasive (i.e. no implants) method of delivering oscillatory stimulation deep in the brain developed by Tsai and Ed Boyden, Y. Eva Tan Professor in the Departments of Biological Engineering and Brain and Cognitive Sciences, the MIT Media Lab and McGovern Institute, and co-director of the MIT Center for Neurobiological Engineering. In June 2017 in Cell they showed they could deliver oscillating electrical fields into tightly focused volumes deep within the brains of mice, for instance to the hippocampus.
The system works by generating high frequency fields –too high to stimulate neurons – from head-mounted electrodes. Importantly, the supplied frequencies differ by exactly the amount to be instilled. Where the waves interfere in the brain, what remains is this difference frequency. In the paper, for example, they generated fields of 2 kHz and 2.01 kHz, yielding a difference frequency of 10 Hz where the waves interfered. In experiments in the paper, they showed that they could reposition where that spot was simply by varying the field strengths.
The team reported several other crucial demonstrations. One was that when they focused on the hippocampus, overlying regions like the cortex remained unaffected. This overcomes a drawback of transcranial magnetic stimulation, a clinically approved brain stimulation technology. Another was that they could use the 10 Hz frequency to affect behavior: By moving the signal around the motor cortex, they compelled mice to move different body parts. Finally, they found no adverse safety effects.
Now they’ll ask whether the technology, called temporal interference (TI), could benefit patients with neurological conditions. Chan, Tsai and Boyden are planning experiments in which TI will treat mouse models of Parkinson’s disease. Essentially they hope to provide DBS non-invasively. Myriam Heiman, Latham Family CD Assistant Professor in the Picower Institute, who studies neurodegenerative diseases, is collaborating. Success in mice and eventually in people could create new treatment possibilities. Chan said more Parkinson’s patients might be able to receive TI than can receive implanted treatment. Boyden added that with a system like TI where the location, frequency and strength of an instilled rhythm can easily be varied, clinicians could tailor treatment more precisely for each patient.
Producing innovations for societal impact, derived from basic research, is a key goal of the Aging Brain Initiative, Tsai said.
Producing innovations for society impact, derived from basic research, is a key goal of the Aging Brain Initaitive, Tsai said.
"One of the main missions is to quickly translate experimental results to patients," Tsai said. “We are very fortunate here to have people from all the different disciplines working together so we can come up with these less traditional types of treatment approaches.”
TI might also have an impact on Alzheimer’s disease, Tsai adds. In December 2016, in a powerful demonstration of the potential of non-invasively manipulating brain rhythms, she, Boyden and Emery Brown, Edward Hood Taplin Professor of Computational Neuroscience and Health Sciences & Technology, discovered that having mice gaze at lights that flicker at 40 Hz – the frequency of a gamma rhythm in the brain – helped Alzheimer’s model mice to reduce the buildup of harmful amyloid beta proteins. The experiments reported in Nature showed that entraining the gamma rhythm in the visual cortex coordinated beneficial activity, for instance increasing the activity of microglia, specialized brain cells that clear away harmful protein plaques. Gamma light flicker therapy has since begun human trials.
Tsai’s lab is interested to learn whether TI can help extend or enhance that effect by delivering gamma frequencies directly to other regions. Tsai’s hope is that gamma therapy can provide an effective Alzheimer’s treatment, especially as drug trials continue to disappoint.
Waves and Cognition
Miller studies the role of rhythms in cognition and working memory, where we exert rapid, volitional control over the information we process. Early in 2018 he showered the field with evidence from experiments in animals that a coordinated byplay of beta and gamma rhythms in the pre-frontal cortex (PFC) enables such functions.
In Nature Communications, his team showed that gamma rhythms appear to modulate readout from working memory, for instance when the stored sensory information is needed for cognition. Beta rhythms, meanwhile, control when gamma is active and appear necessary for gating access to, and clearing out, working memory for storing new information. In the Proceedings of the National Academy of Sciences, Miller’s lab showed that the rhythms emerge during working memory tasks in distinct layers of the (PFC): Gamma operates among neurons in superficial cortical layers while beta operates among neurons in the deep layers. This fits with known anatomy, he said: Deep layers carry “feedback” from higher-level to lower level cortex so they are where a beta control signal would be expected. The superficial layers carry “feedforward” sensory information from the outside world and contain sensory-related gamma rhythms.
In Neuron, Miller’s group examined the role of rhythms amid the task of sorting images into relatively literal or abstract categories. Monkeys employed different rhythms in different areas of the cortex: The literal thinking involved entraining gamma in the ventral PFC, while more abstract thinking came about with bursts of beta rhythms in the dorsal PFC.
Miller, too, is considering how non-invasive brainwave manipulation could help patients with psychiatric conditions, such as in autism or schizophrenia, where working memory or reasoning may be aberrant. Another idea might be to intervene to enhance alpha and beta rhythms to modulate attention, Miller said.
“Let’s say you have a brain that is having trouble focusing attention and top-down control,” he said. “That depends, according to our new model, on alpha and beta rhythms. If you could strengthen those, in theory, you could improve people’s ability to stay on task.”
The ability to evaluate such questions depends on the insights and technologies that Picower Institute scientists have developed. How might it enhance health to look beyond the brain’s anatomy to its rhythmic activity? Stay tuned to these frequencies.