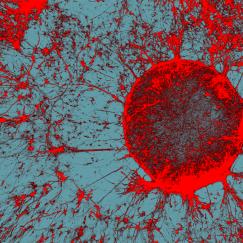
Bringing complementary skills to a shared mission as part of MIT’s Aging Brain Initiative, the team seamlessly blends and advances some of the hottest and most powerful methods in science – statistical genetics, computational genomics, epigenomics, machine learning, single-cell profiling, “big data” integration, induced stem-cell reprogramming, mini-brain organoids, tissue engineering, and CRISPR-Cas9 genetic manipulation.
This allows their teams to study genetic and molecular differences between healthy and diseased samples from multiple brain regions of humans and mice, integrate and analyze the resulting data to identify significant disease-driver genes and the cell types where they act, and engineer cells, tissues and mouse models to test their hypotheses and discover therapeutic interventions.
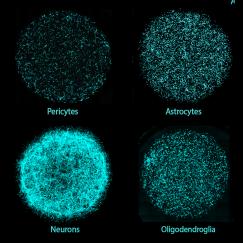
“Working together, we have the opportunity to garner big data from a large number of human subjects to elucidate the driver genes and pathways that are novel but key to the disease,” said Tsai, Picower Professor and director of the Picower Institute for Learning and Memory. “We can then test these genes/pathways in the induced pluripotent stem cells (iPSC) system coupled with CRISPR-Cas9 to manipulate the genome. We can induce the iPS cells into all major brain cell types, and dissect the contributions of each of these cell types to disease.”
It’s a joint research venture that’s as close, cutting-edge, and multidisciplinary as any at MIT, and fits squarely within the Schwarzman College of Computing’s emphasis on integrating artificial intelligence with the sciences. Kellis recalls it all getting started back in 2012 via the connection of postdocs, Elizabeth Gjoneska of the Tsai Lab and Andreas Pfenning from the Kellis Lab, who had met at a seminar on campus. With similarly overlapping interests in how gene regulation, and specifically epigenomic differences, affect the workings and health of the brain, they and other members of the two labs kindled dialogues that soon brought the professors together.
“The collaboration kind of happened organically,” said Kellis, professor of computer science and head of MIT’s Computational Biology Group. “We found kindred spirits – folks who thought similarly but were extremely complementary in their expertise.”
Within two years, the labs had jointly published two major papers. One in Nature, part of a sweeping set of reports on epigenomics that Kellis helped lead, showed that highly analogous sets of gene misregulation signals in the hippocampus of mice and humans each revealed a strong role for the brain’s immune cells and processes in allowing Alzheimer’s disease to progress. The other paper, in Cell, showed that in order to rapidly express genes critical for experience to affect synaptic connections, neurons naturally employ double-strand breaks of their DNA. The team hypothesized that failure to repair these breaks increases with age and may also contribute to neurodegeneration.
Each paper demonstrated the power of their combined approach. Since then, the collaboration has grown significantly to encompass about half a dozen projects. In 2016, for instance, they earned a National Institutes of Health grant to determine the significant epigenomic differences afoot in major brain cell types in Alzheimer’s disease.
In the last year, Kellis and Tsai received an influx of several new NIH grants and philanthropic gifts, enabling them to substantially expand their efforts in Alzheimer’s, tackle new disorders, bring in new collaborators, include new types of experiments, and expand their mechanistic studies. Their new directions include Schizophrenia, Bipolar Disorder, Psychosis in Alzheimer’s Disease, Frontotemporal Dementia, Lewy Body Dementia, and healthy aging.
Importantly, each experiment is designed together, Kellis says. Knowing that the team combines the capabilities of each lab, the team can be more ambitious.
“We think in a different way than any one lab would think by itself,” Kellis said. “For instance, I wouldn’t have the guts to ask many of these things that we are asking, if it wasn’t for our close collaboration with Li-Huei’s lab.”
With the new NIH grants, they will ask a litany of questions such as why many people with Alzheimer’s develop psychotic symptoms as well, what are the unique molecular signatures that distinguish Alzheimer’s and other dementias, and how do specific genetic variations in non-coding DNA elevate risk for a number of neurodegenerative and neuropsychiatric disorders.
“How privileged I feel to work with the world’s best computational team,” Tsai said. “This is only possible at MIT.”