The degree to which a surgical patient’s subconscious processing of pain, or “nociception,” is properly managed by their anesthesiologist will directly affect the degree of post-operative drug side effects they’ll experience and the need for further pain management they’ll require. But pain is a subjective feeling to measure, even when patients are awake, much less when they are unconscious. In a new study, MIT and Massachusetts General Hospital (MGH) researchers describe a set of statistical models that objectively quantified nociception during surgery. Ultimately, they hope to help anesthesiologists optimize drug dose and minimize post-operative pain and side effects.
The new models integrate data meticulously logged over 18,582 minutes of 101 abdominal surgeries in men and women at MGH. Led by former MIT graduate student Sandya Subramanian, now an assistant professor at UC Berkeley and UC San Francisco, the researchers collected and analyzed data from five physiological sensors as patients experienced a total of 49,878 distinct “nociceptive stimuli” (such as incisions or cautery). Moreover, the team recorded what drugs were administered, and how much and when, to factor in their effects on nociception or cardiovascular measures. They then used all the data to develop a set of statistical models that performed well in retrospectively indicating the body’s response to nociceptive stimuli.
The team’s goal is to furnish such accurate, objective, and physiologically principled information in real-time to anesthesiologists who currently have to rely heavily on intuition and past experience in deciding how to administer pain-control drugs during surgery. If anesthesiologists give too much, patients can experience side effects ranging from nausea to delirium. If they give too little, patients may feel excessive pain after they awaken.
“Sandya’s work has helped us establish a principled way to understand and measure nociception (unconscious pain) during general anesthesia,” said study senior author Emery N. Brown, Edward Hood Taplin Professor of Medical Engineering and Computational Neuroscience in The Picower Institute for Learning and Memory, the Institute for Medical Engineering and Science, and the Department of Brain and Cognitive Sciences at MIT. Brown is also an anesthesiologist at MGH and a Professor at Harvard Medical School. “Our next objective is to make the insights that we have gained from Sandya’s studies reliable and practical for anesthesiologists to use during surgery.”
Surgery and statistics
The research, publsihed in the Proceedings of the National Academy of Sciences, began as Subramanian’s doctoral thesis project in Brown’s lab in 2017. The best prior attempts to objectively model nociception have either relied solely on the electrocardiogram (ECG, an indirect indicator of heart-rate variability) or other systems that may incorporate more than one measurement, but were either based on lab experiments using pain stimuli that do not compare in intensity to surgical pain or were validated by statistically aggregating just a few time points across multiple patients’ surgeries, Subramanian said.
“There’s no other place to study surgical pain except for the operating room,” Subramanian said. “We wanted to not only develop the algorithms using data from surgery, but also actually validate it in the context in which we want someone to use it. If we are asking them to track moment-to-moment nociception during an individual surgery, we need to validate it in that same way.”
So she and Brown worked to advance the state of the art by collecting multi-sensor data during the whole course of actual surgeries and by accounting for the confounding effects of the drugs administered. In that way, they hoped to develop a model that could make accurate predictions that remained valid for the same patient all the way through their operation.
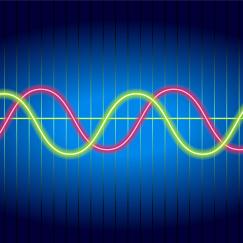
Part of the improvements the team achieved arose from tracking patterns of heart rate and also skin conductance. Changes in both of these physiological factors can be indications of the body’s primal “fight or flight” response to nociception or pain, but some drugs used during surgery directly affect cardiovascular state, while skin conductance (or “EDA,” electrodermal activity) remains unaffected. The study measures not only ECG but also backs it up with PPG, an optical measure of heart rate (like the oxygen sensor on a smartwatch), because ECG signals can sometimes be made noisy by all the electrical equipment buzzing away in the operating room. Similarly, Subramanian backstopped EDA measures with measures of skin temperature to ensure that changes in skin conductance from sweat were because of nociception and not simply the patient being too warm. The study also tracked respiration.
Then the authors performed statistical analyses to develop physiologically relevant indices from each of the cardiovascular and skin conductance signals. And once each index was established, further statistical analysis enabled tracking the indices together to produce models that could make accurate, principled predictions of when nociception was occurring and the body’s response.
Nailing nociception
In four versions of the model, Subramanian “supervised” them by feeding them information on when actual nociceptive stimuli occurred so that they could then learn the association between the physiological measurements and the incidence of pain-inducing events. In some of these trained versions she left out drug information and in some versions she used different statistical approaches (either “linear regression” or “random forest”). In a fifth version of the model, based on a “state space” approach, she left it unsupervised, meaning it had to learn to infer moments of nociception purely from the physiological indices. She compared all five versions of her model to one of the current industry standards, an ECG-tracking model called ANI.
Each model’s output can be visualized as a graph plotting the predicted degree of nociception over time. ANI performs just above chance but is implemented in real time. The unsupervised model performed better than ANI, though not quite as well as the supervised models. The best performing of those was one that incorporated drug information and used a “random forest” approach. Still, the authors note, the fact that the unsupervised model performed significantly better than chance suggests that there is indeed an objectively detectable signature of the body’s nociceptive state even when looking across different patients.
“A state space framework using multisensory physiological observations is effective in uncovering this implicit nociceptive state with a consistent definition across multiple subjects,” wrote Subramanian, Brown and their co-authors. “This is an important step toward defining a metric to track nociception without including nociceptive ‘ground truth’ information, most practical for scalability and implementation in clinical settings.”
Indeed the next steps for the research are to increase the data sampling and to further refine the models so that they can eventually be put into practice in the operating room. That will require enabling them to predict nociception in real-time, rather than in post-hoc analysis. When that advance is made, that will enable anesthesiologists or intensivists to inform their pain drug dosing judgements. Further into the future, the model could inform closed-loop systems that automatically dose drugs under the anesthesiologist’s supervision.
“Our study in an important first step toward developing objective markers to track surgical nociception,” the authors concluded. “These markers will enable objective assessment of nociception in other complex clinical settings, such as the ICU, as well as catalyze future development of closed-loop control systems for nociception.”
In addition to Subramanian and Brown, the paper’s other authors are Bryan Tseng, Marcela del Carmen, Annekathryn Goodman, Douglas Dahl and Riccardo Barbieri.
Funding from The JPB Foundation, The Picower Institute for Learning and Memory, George J. Elbaum (MIT '59, SM '63, PhD '67), Mimi Jensen, Diane B. Greene (MIT, SM '78), Mendel Rosenblum, Bill Swanson, Cathy and Lou Paglia, annual donors to the Anesthesia Initiative Fund, the National Science Foundation and an MIT Office of Graduate Education Collabmore-Rogers Fellowship supported the research.